Fracture Analysis and Failure Mechanism of TA3 Limited Contact-Dynamic Compression Plates
-
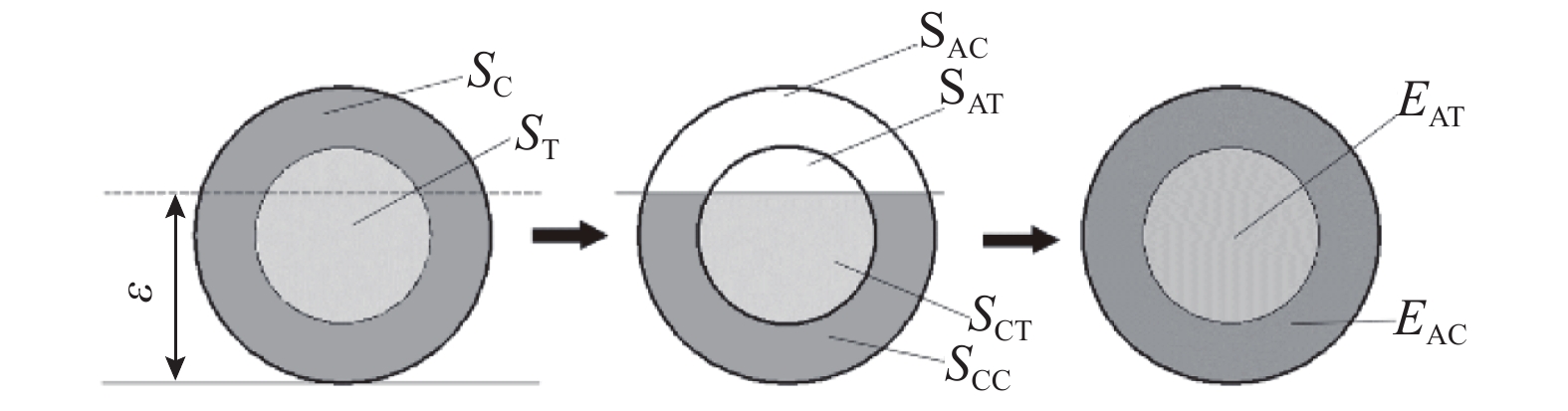
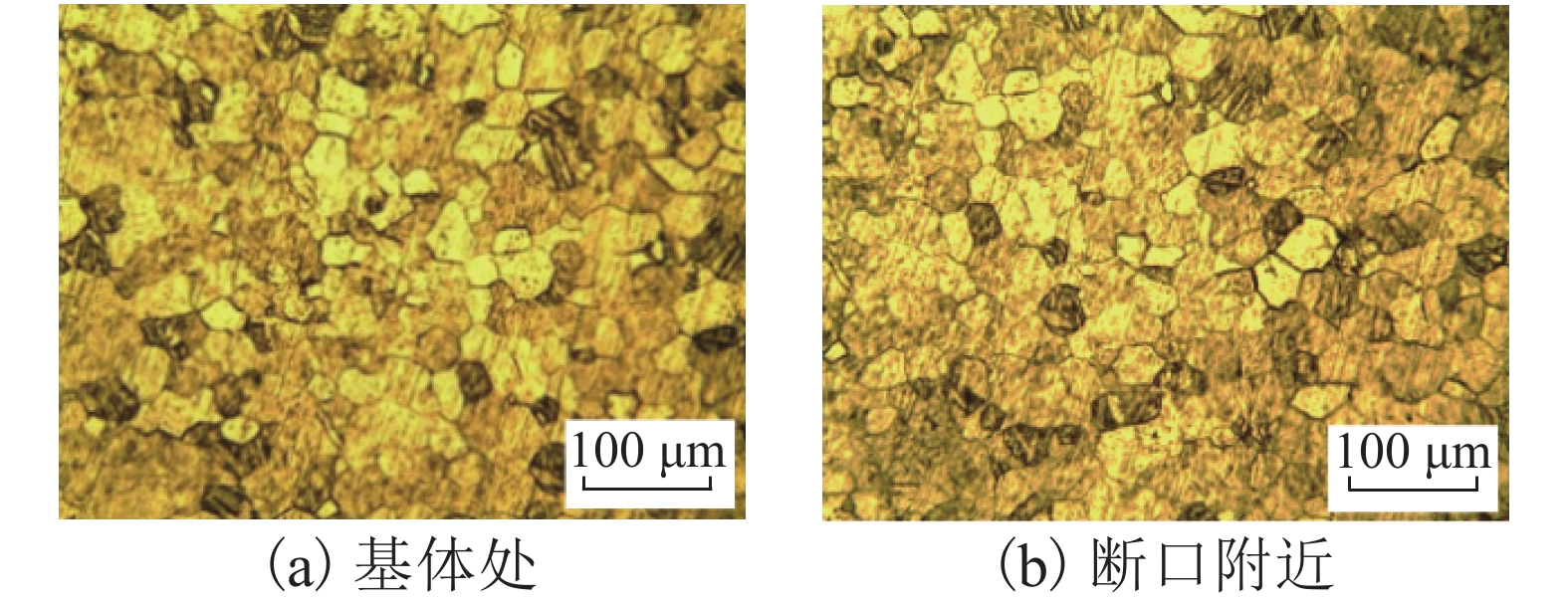
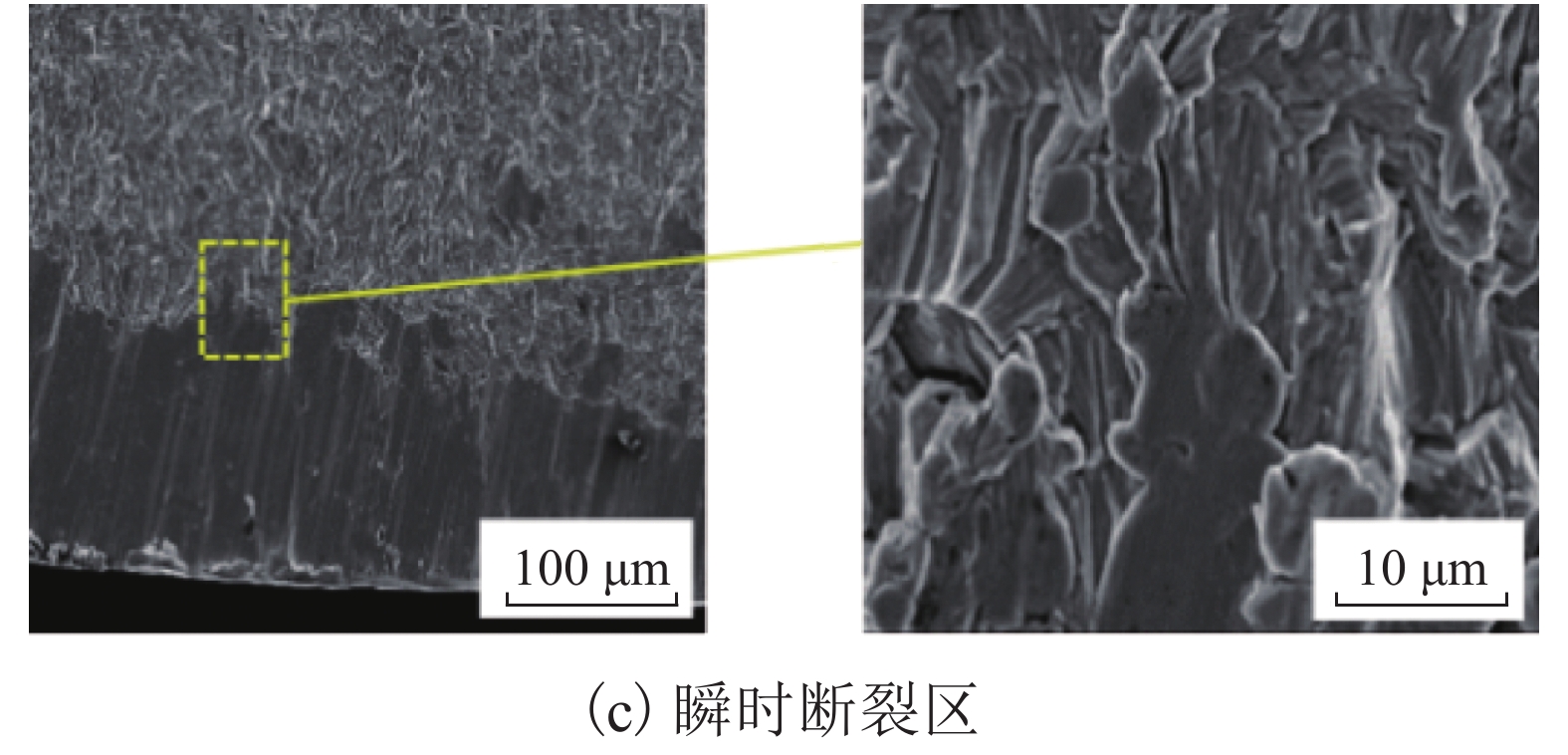
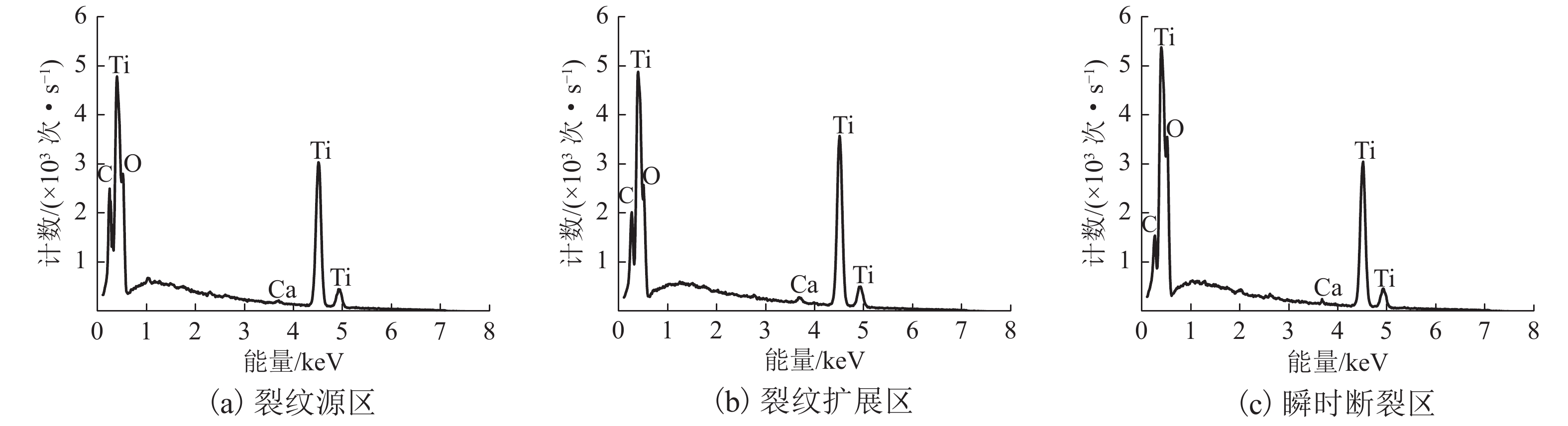
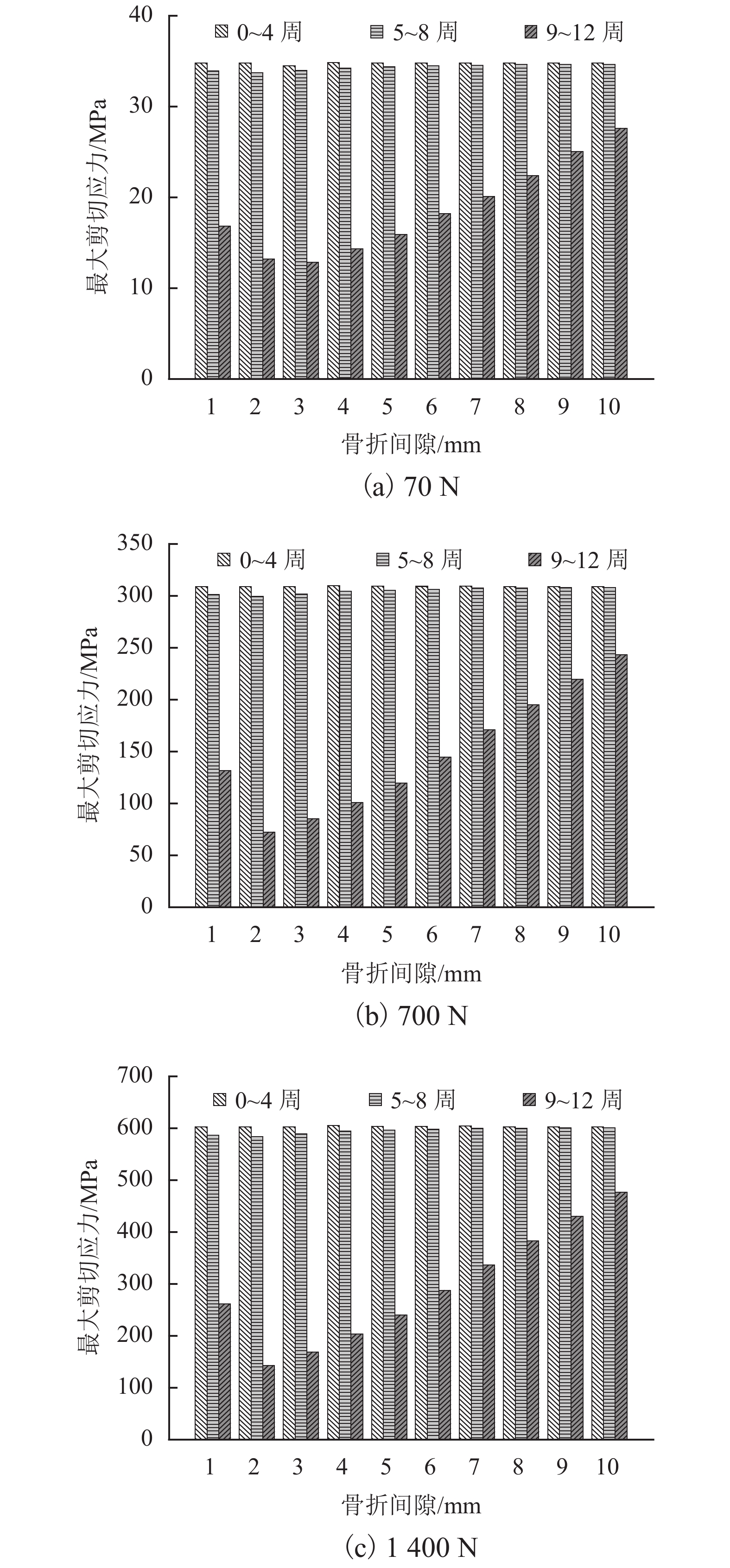
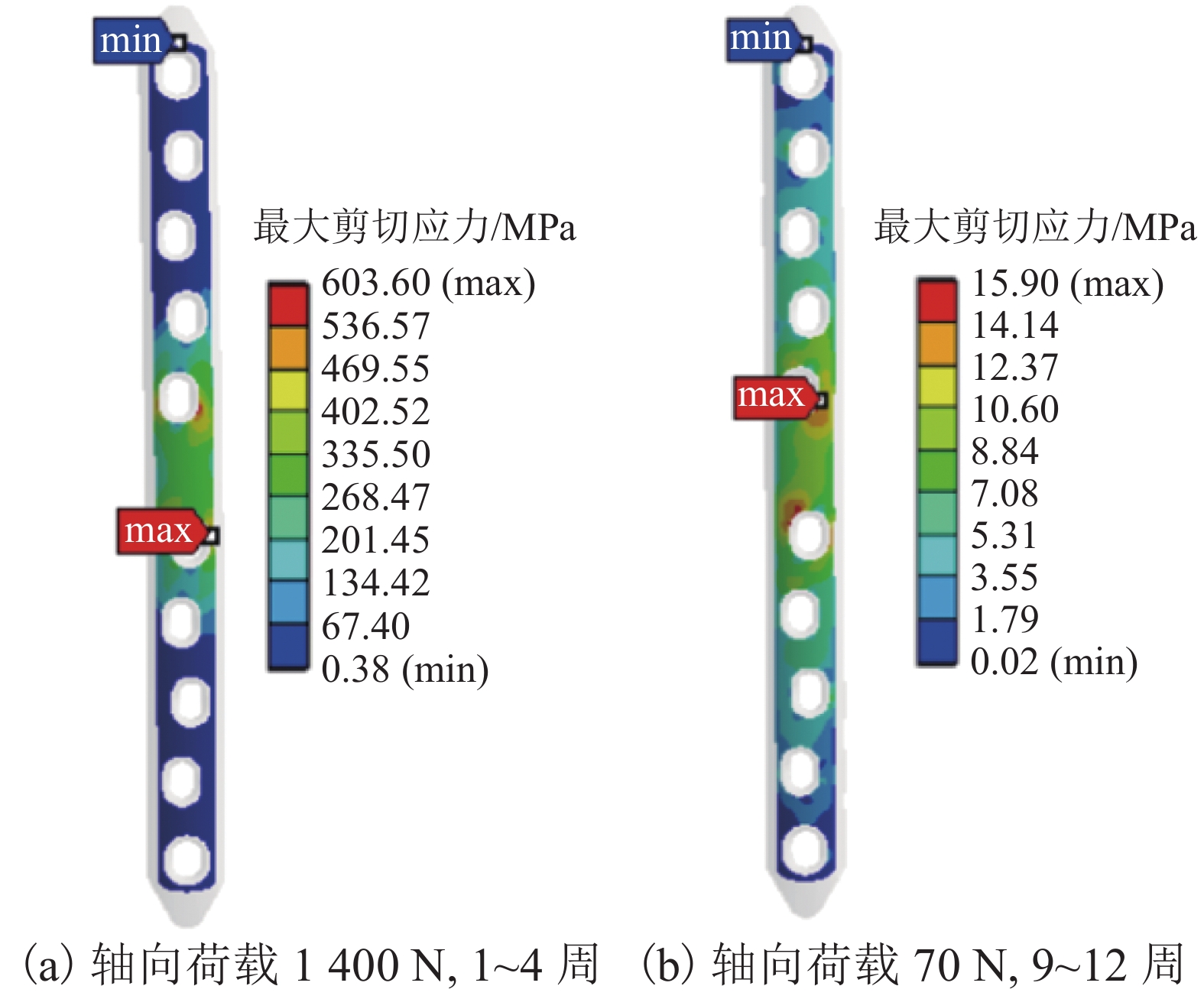
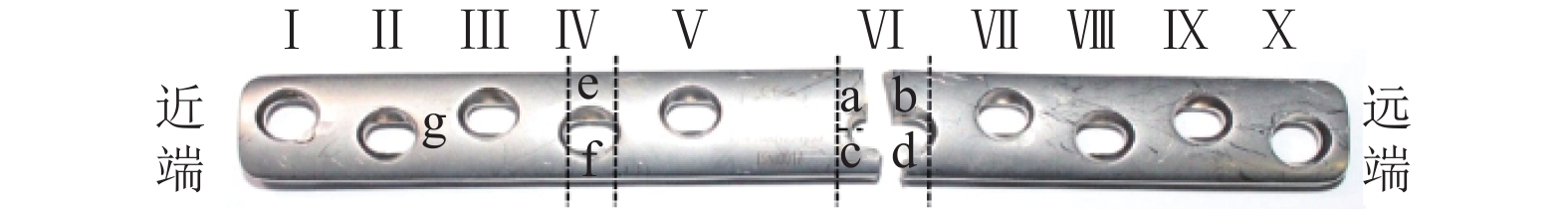
摘要: 为探究TA3纯钛有限接触动态加压接骨板(LC-DCP)在人体内服役期间发生断裂的失效机制,采用化学成分分析仪、维氏硬度仪、光学显微镜和扫描电镜(SEM)等手段,对7个临床断裂失效的TA3纯钛LC-DCP样品进行了断口形貌分析;建立了TA3纯钛LC-DCP固定股骨干中段横形骨折的三维有限元模型,并采用ANSYS对该模型进行了受力分析. 研究结果表明:7个TA3纯钛LC-DCP样品的材料符合要求,断口均位于接骨板中段螺钉孔处;断口表面均出现疲劳辉纹和二次裂纹,裂纹源区、扩展区和瞬时断裂区的元素组成相同;骨折患者在愈合前下地行走会导致接骨板的最大剪切应力大于TA3材料的屈服强度极限,且最大剪切应力发生在接骨板中段螺钉孔处;TA3纯钛LC-DCP的临床断裂失效主要源于骨折患者在愈合前下地行走导致过载,使得接骨板中段螺钉孔处萌生裂纹,随后承受循环疲劳载荷,最终断裂失效.Abstract: To investigate the fracture mechanism of TA3 pure titanium limited contact-dynamic compression plates (LC-DCP) during service in the body. 7 clinically fractured TA3 pure titanium LC-DCP were collected and sterilized, and their fracture surfaces were examined using chemical composition analyzer, Vickers hardness tester, optical microscope, and scanning electron microscope. A three-dimensional finite element model of middle femoral transverse fracture treated by TA3 pure titanium LC-DCP was established, and then the fracture healing and bone plate stress were analyzed using ANSYS software. The results show that the physical and chemical properties of the 7 LC-DCP are qualified, fracture occurs around the middle screw hole on the bone plates. Fatigue striations and secondary cracks appear on the fracture surface, and the regions of crack initiation, propagation and transient fracture, have same elemental compositions. For the patients walking prematurely, the maximum shear stress of bone plates occurs at the middle screw hole and it exceeds the yield strength of TA3 pure titanium. In sum, the fracture failure of the TA3 pure titanium LC-DCP in body is mainly resulted from patients walking prematurely, at the condition, cracks are initiated at the middle screw hole on the bone plate surface, and fatigue fracture occurs under the action of complex cyclic loading.
-
Key words:
- bone plate /
- facture analysis /
- finite element analysis /
- fatigue crack /
- failure analysis
-
表 1 股骨和TA3纯钛的材料参数
Table 1. Material parameters of femur and TA3 pure titanium
对象 弹性模量/GPa 泊松比 皮质骨 Ex (纵向)= 18.400
Ey (横向) = 7.000
Ez (径向) = 8.500νxy (xy 面)= 0.120
νyz (yz 面)= 0.370
νxz (xz 面)= 0.140松质骨 1.061 0.225 TA3纯钛 103.400 0.300 表 2 TA3纯钛LC-DCP的化学成分(质量分数)
Table 2. Chemical compositions of TA3 pure titanium LC-DCP (mass)
% 样品编号 C N O H Fe 1# 0.0016 0.0067 0.2072 0.0012 0.2081 2# 0.0030 0.0129 0.1637 0.0009 0.0701 3# 0.0023 0.0151 0.2093 0.0011 0.1673 4# 0.0106 0.0116 0.1196 0.0012 0.2543 5# 0.0116 0.0068 0.1879 0.0005 0.2008 6# 0.0020 0.0197 0.2186 0.0001 0.1798 7# 0.0101 0.0161 0.2721 0.0069 0.2500 标准值 ≤0.0800 ≤0.0500 ≤0.3500 ≤0.0150 ≤0.3000 表 3 TA3纯钛DCP接骨板的维氏硬度(HV10)
Table 3. Vickers hardness of TA3 pure titanium DCP bone plates (HV10)
样品编号 断口 基体 标准值 均值 最大偏差 均值 最大偏差 1# 262 15 260 11 ≥ 150 2# 270 18 273 16 3# 243 9 248 10 4# 273 13 265 10 5# 225 16 230 18 6# 271 13 266 12 7# 220 15 225 13 表 4 TA3纯钛LC-DCP接骨板的平均晶粒度
Table 4. Averaged grain size of TA3 pure titanium LC-DCP bone plates
样品编号 断口处 基体处 标准值 1# 7.18 7.10 ≥ 5.00 2# 9.21 9.20 3# 8.66 8.59 4# 8.48 8.37 5# 7.00 6.95 6# 9.24 9.21 7# 9.67 9.60 表 5 术后4周、8周中间骨痂的材料属性
Table 5. Calculated material properties of the callus 4 and 8 weeks after surgery
骨折间
隙/mm4 周皮质骨 4 周松质骨 8 周皮质骨 8 周松质骨 弹性模
量/MPa愈合效
率/%弹性模
量/MPa愈合效
率/%弹性模
量/MPa愈合效
率/%弹性模
量/MPa愈合效
率/%1 0.06 9.54 0 0 3.79 13.35 0 0 2 0.17 83.90 0.01 100.00 25.60 91.36 1.65 100.00 3 0.19 100.00 0.01 100.00 28.00 100.00 1.65 100.00 4 0.19 99.57 0.01 100.00 27.22 97.20 1.65 100.00 5 0.18 90.06 0.01 100.00 24.91 88.89 1.65 100.00 6 0.16 75.98 0.01 100.00 20.89 74.46 1.65 100.00 7 0.14 63.14 0.01 86.71 17.25 61.40 1.36 82.60 8 0.12 51.76 0.01 57.11 14.14 50.27 0.87 52.89 9 0.11 41.35 0.01 28.30 11.06 39.24 0.38 22.89 10 0.09 30.31 0 3.98 8.17 28.94 0.04 2.09 -
OESTERN H J, TRENTZ O, URANUES S. Bone and joint injuries: trauma surgery Ⅲ[M]. Berlin : Springer, 2014: 265-296. 谯波,蒋电明. 接骨板材料的研究现状[J]. 重庆医科大学学报,2017,42(2): 62-66.QIAO Bo, JIANG Dianming. Research in materials for bone plate[J]. Journal of Chongqing Medical University, 2017, 42(2): 62-66. 王荣,杨星红. 人体主股骨接骨板断裂失效分析[J]. 腐蚀科学与防护技术,2013,25(6): 504-507.WANG Rong, YANG Xinghong. Failure analysis of a fracturd of bone connection plate of TA3 for body’s main femur[J]. Corrosion Science and Protection Technology, 2013, 25(6): 504-507. 李荣,魏东,许陆,等. 外科植入用TA3钛合金接骨板断裂失效分析[J]. 理化检验(物理分册),2016,52(12): 897-899.LI Rong, WEI Dong, XU Lu, et al. Fracture failure analysis of TA3 titanium alloy blade plates for surgical implants[J]. Physical Testing and Chemical Analysis (Part A:Physics Testing), 2016, 52(12): 897-899. 周梦林. 镁合金接骨板的力学性能与微动磨损特性研究[D]. 成都: 西南交通大学, 2017. AZEVEDO C R F, HIPPERT E. Failure analysis of surgical implants in Brazil[J]. Engineering Failure Analysis, 2002, 9(6): 621-633. doi: 10.1016/S1350-6307(02)00026-2 AZEVEDO C R F. Failure analysis of a commercially pure titanium plate for osteosynthesis[J]. Engineering Failure Analysis, 2003, 10(2): 153-164. doi: 10.1016/S1350-6307(02)00067-5 GHIBAN B, VARLAN F C, NIVULESCU M, et al. Fractographic evaluation of the metallic materials for medical applications[J]. Key Engineering Materials, 2017, 745(3): 62-74. PROVERBIO E, BONACCORSI L M. Microstructural analysis of failure of a stainless steel bone plate implant[J]. Practical Failure Analysis, 2001, 1(4): 33-38. doi: 10.1007/BF02715331 KANCHANIMAI C, PHIPHOBMONGKOL V, MUANJAN P. Fatigue failure of an orthopedic implant—a locking compression plate[J]. Engineering Failure Analysis, 2008, 15(5): 521-530. doi: 10.1016/j.engfailanal.2007.04.001 MARCOMINI J B, BAPTISTA C A R P, PASCON J P, et al. Investigation of a fatigue failure in a stainless steel femoral plate[J]. Journal of the Mechanical Behavior of Biomedical Materials, 2014, 38(38): 52-58. TAVARES S S M, MAINIER F B, ZIMMERMAN F, et al. Characterization of prematurely failed stainless steel orthopedic implants[J]. Engineering Failure Analysis, 2010, 17(5): 1246-1253. doi: 10.1016/j.engfailanal.2010.02.003 NIRAJAN T, PRAYSON M, GOSWAMI T. A failure study of a locking compression plate implant[J]. Case Studies in Engineering Failure Analysis, 2015, 3(4): 68-72. GERVAIS B, VADEAN A, RAISON M, et al. Failure analysis of a 316L stainless steel femoral orthopedic implant[J]. Case Studies in Engineering Failure Analysis, 2016, 5: 30-38. MEHBOOB H, CHANG S H. Application of composites to orthopedic prostheses for effective bone healing:a review[J]. Composite Structures, 2014, 118(1): 328-341. KIM S H, CHANG S H, JUNG H J. The finite element analysis of a fractured tibia applied by composite bone plates considering contact conditions and time-varying properties of curing tissues[J]. Composite Structures, 2010, 92(9): 2109-2118. doi: 10.1016/j.compstruct.2009.09.051 KIM H J, CHANG S H, JUNG H J. The simulation of tissue differentiation at a fracture gap using a mechano-regulation theory dealing with deviatoric strains in the presence of a composite bone plate[J]. Composites Part B, 2012, 43(3): 978-987. doi: 10.1016/j.compositesb.2011.09.011 KIM H J, KIM S H, CHANG S H. Bio-mechanical analysis of a fractured tibia with composite bone plates according to the diaphyseal oblique fracture angle[J]. Composites Part B, 2011, 42(4): 666-674. doi: 10.1016/j.compositesb.2011.02.009 HEINTZ S, GUTIERREZ-FAREWIK E M. Static optimization of muscle forces during gait in comparison to EMG-to-force processing approach[J]. Gait & Posture, 2007, 26(2): 279-288. PERREN S M. Evolution of the internal fixation of long bone fractures[J]. The Journal of Bone and Joint Surgery, 2002, 84(8): 1093-110. doi: 10.1302/0301-620X.84B8.0841093 GANESH V K, RAMAKRISHNA K, GHISTA D N. Biomechanics of bone-fracture fixation by stiffness-graded plates in comparison with stainless-steel plates[J]. Bio-Medical Engineering Online, 2005, 4(1): 46-60. MEHBOOB H, SON D S, CHANG S H. Finite element analysis of tissue differentiation process of a tibia with various fracture configurations when a composite intramedullary rod was applied[J]. Composites Science & Technology, 2013, 80(6): 55-65. 孙训方, 方孝淑, 关来泰. 材料力学[M]. 北京: 高等教育出版社, 2009: 243-248. 郑照县. 股骨骨折内固定金属接骨板的生物力学性能研究[D]. 成都: 西南交通大学, 2017. GARDNER T N, STOLL T. The influence of mechanical stimulus on the pattern of tissue differentiation in a long bone fracture–an FEM study[J]. Biomechanics, 2000, 33(4): 415-25. doi: 10.1016/S0021-9290(99)00189-X PINTO C M S A, ASPRINO L, DE MORAES M. Chemical and structural analyses of titanium plates retrieved from patients[J]. International Journal of Oral & Maxillofacial Surgery, 2015, 44(8): 1005-1009. -




 下载:
下载: